Features
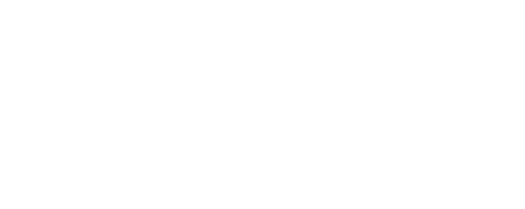
AI-Powered VOB
Our AI agents automatically communicate with the payers, agents around the benefit verification. If something goes wrong, a human steps into the process.
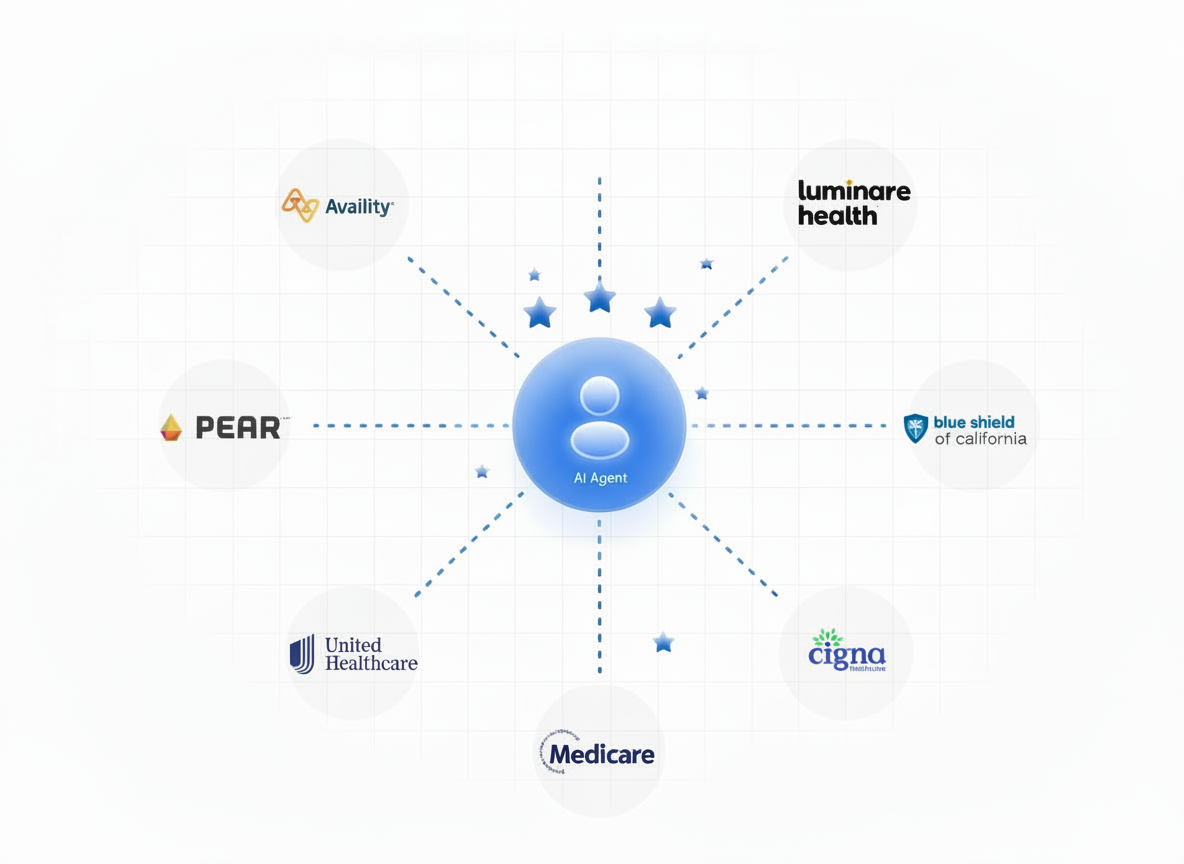
Real-time patient response
Your patients can see their coverage and out-of-pocket patient responsibility immediately, instead of waiting for you to pull them back.
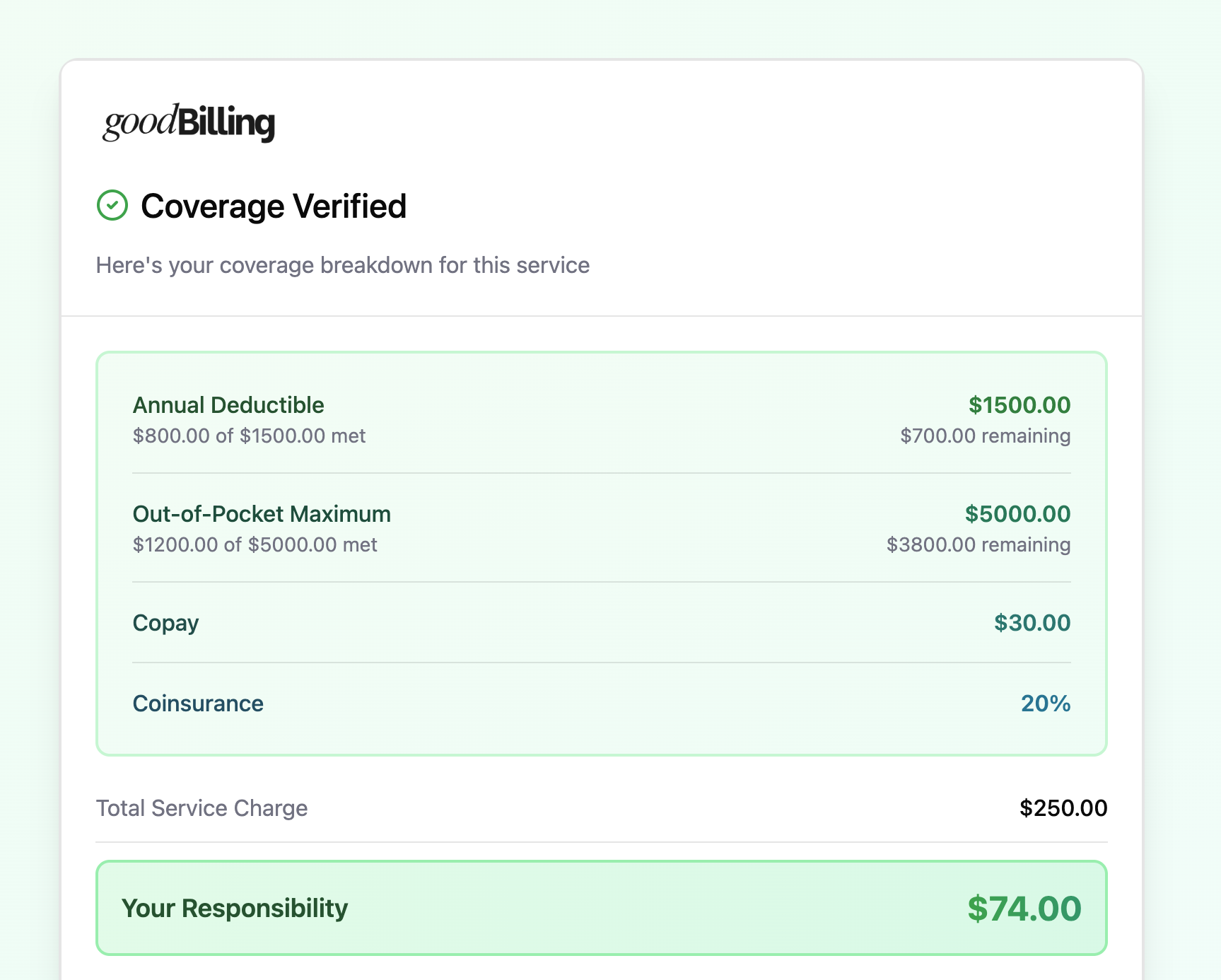

Full end-to-end EMR integration
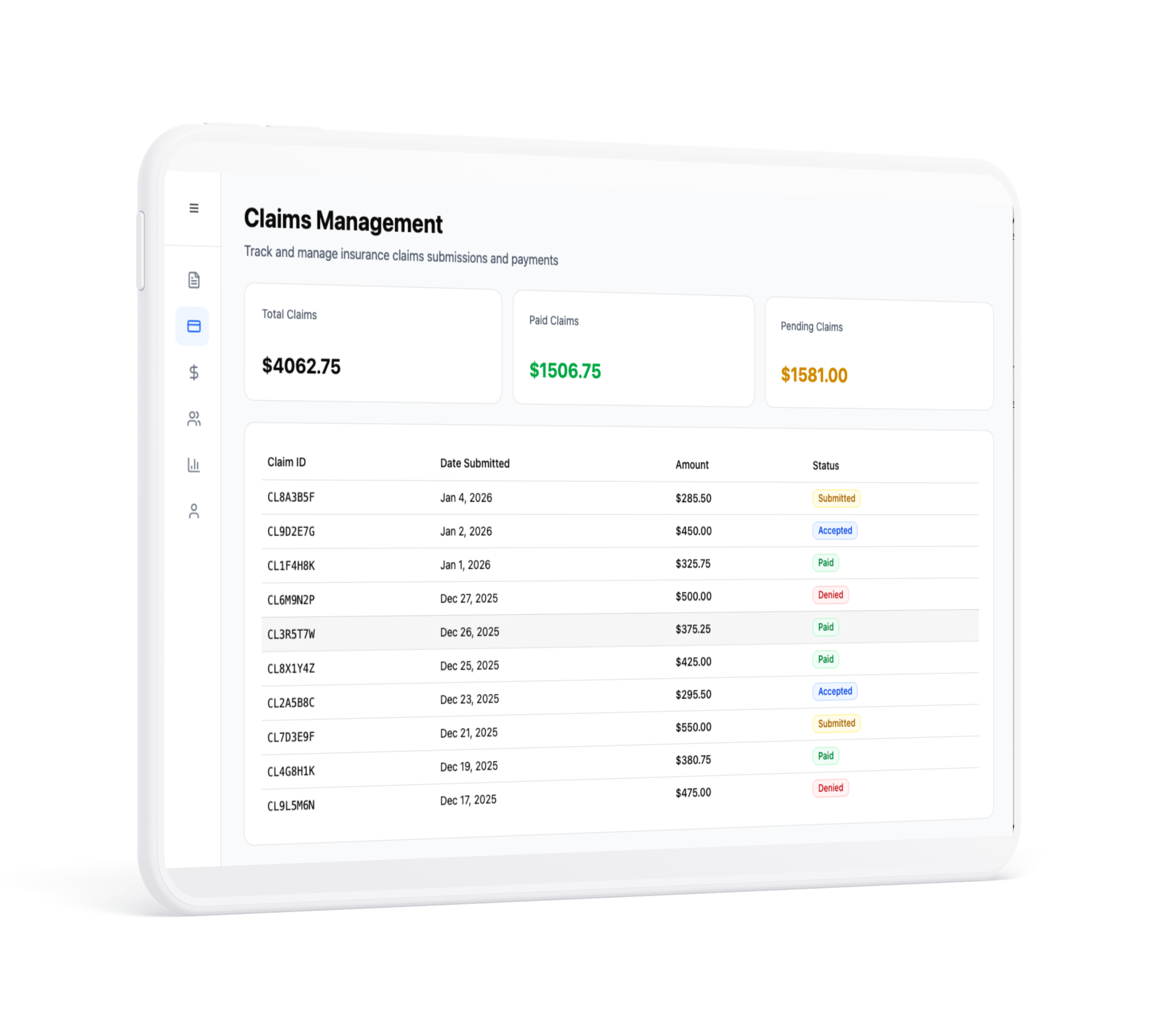
We post policy and claim level information to your EMR automatically. Claims are created as soon as an appointment is over.
AI powered claim generation
Our AI uses information, medical records, clinical notes, as well as recorded diagnoses for the patient to create accurate claims and minimize denials.
Features that work for you
Automated reminders
Reduce no-shows with automated text, email, and phone reminders sent to patients.
Predictive analytics
Identify at-risk patients and forecast outcomes based on historical health data.
.webp)
Inventory management
Track medical supplies, medications, and equipment in real-time to maintain adequate.
GoodBilling vs Traditional RCM
Lower costs
VOBs are free and we charge a much lower percentage of claim for the service. We only charge for successfully adjudicated claims
Faster turnaround
By automating many steps of the process we substantially shorten the payment cycle
Automatic rules updates
We track changes in patient's coverage as well as changes in payer contracts and update the billing logic accordingly
HIPAA compliance
We reduce the scope of manual intervention and store information in secure HIPAA compliant environment.
Conversion boost
By offering your patients the ability to check their coverage and responsibility in real time, you increase patient conversion from your practice website.
EMR integration
We rely on direct EMR integrations versus a biller going into your EMR system and pulling records manually.
Experience the future of RCM
Talk to us today and see how goodBilling can help your practice.

.svg)